Peter Insio Wang 认为,肿瘤细胞非常“狡猾”。它们会用各种阴险的手段逃避人体免疫系统对抗这些癌症入侵者的免疫反应。肿瘤细胞会表达程序性死亡配体 1 (PD-L1) 分子,这些分子会像一道保护盾,抑制人体的免疫细胞,从而给靶向癌症免疫疗法带来障碍。
王教授是生物医学工程系阿尔弗雷德·曼教授和德怀特·C和希尔达加德·E·鲍姆教授,他领导的实验室致力于开创性地研究工程免疫疗法,利用人类免疫系统打造未来抗击癌症的武器库。
王氏实验室的研究人员开发出一种新方法,可以将肿瘤细胞的阴险防御机制转向自身,将这些“屏蔽”分子转变为王氏实验室设计的嵌合抗原受体 (CAR) T 细胞的靶标,用于攻击癌症。
这项研究由王实验室的博士后研究员朱灵山与王、研究科学家刘龙伟及其合著者共同完成,发表在《ACS Nano》杂志上。
嵌合抗原受体 (CAR) T 细胞疗法是一种革命性的癌症治疗方法,该方法将患者体内的 T 细胞(一种白细胞)提取出来,并注入独特的嵌合抗原受体 (CAR)。CAR 可以与癌细胞相关的抗原结合,引导 T 细胞杀死癌细胞。
王实验室的最新研究成果是设计一种用于 CAR T 细胞的单体,研究小组将其称为 PDbody,它可以与癌细胞上的 PD-L1 蛋白结合,使 CAR 能够识别肿瘤细胞并阻断其防御。
王教授说:“把CAR想象成一辆真正的汽车。它有发动机和油箱,但也有刹车。本质上,发动机和油箱推动CAR-T向前移动并杀死肿瘤。而PD-L1就像刹车一样,阻止了CAR-T的移动。”
在这项工作中,朱、刘、王和团队对 T 细胞进行了设计,以阻断这种抑制“制动”机制,并使 PD-L1 分子成为破坏的目标。
“这种嵌合PDbody-CAR分子可以让我们的CAR-T细胞攻击、识别并杀死肿瘤。同时,它也会阻断肿瘤细胞,阻止CAR-T细胞的攻击。这样,我们的CAR-T细胞就会更加强大。”王教授说。
CAR-T细胞疗法对白血病等“湿性”癌症最有效。研究人员面临的挑战是开发能够区分癌细胞和健康细胞的先进CAR-T细胞。
王的实验室正在探索将该技术靶向肿瘤的方法,以便在肿瘤部位激活 CAR T 细胞,而不会影响健康组织。
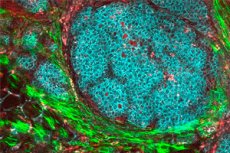
在这项研究中,研究团队专注于一种表达PD-L1蛋白的高侵袭性乳腺癌。然而,PD-L1也由其他类型的细胞表达。因此,研究人员观察了独特的肿瘤微环境——肿瘤周围的细胞和基质——以确保他们设计的PDbody能够更特异性地与癌细胞结合。
朱教授说:“我们知道肿瘤微环境的pH值相对较低,略带酸性。因此,我们希望我们的PDbody在酸性微环境中具有更好的结合能力,这将有助于我们的PDbody区分肿瘤细胞和其他周围细胞。”
为了提高治疗的精准度,研究团队使用了一种名为 SynNotch 的基因“门控”系统,该系统可确保带有 PDbody 的 CAR T 细胞仅攻击表达不同蛋白质 CD19 的癌细胞,从而降低损害健康细胞的风险。
“简而言之,得益于这个SynNotch门控系统,T细胞只会在肿瘤部位被激活,”朱教授说。“不仅pH值更酸性,而且肿瘤细胞表面也会决定T细胞是否被激活,这给了我们两个层面的控制。”
朱指出,研究团队使用了小鼠模型,结果显示,SynNotch门控系统指导带有PDbody的CAR-T细胞仅在肿瘤部位激活,杀死肿瘤细胞,同时对动物的其他部位保持安全。
受进化启发的 PDbody 创建过程
该团队运用计算方法,并从进化过程中汲取灵感,创造出了专门的PDbodies。定向进化是生物医学工程中用于在实验室环境中模拟自然选择过程的一种技术。
研究人员创建了一个定向进化平台,其中包含他们设计的蛋白质的庞大迭代库,以发现哪个版本可能最有效。
王说:“我们需要创造一些东西来识别肿瘤表面的 PD-L1。”
“我们利用定向进化,筛选出大量不同的单体突变,以确定哪一个能够与PD-L1结合。选定的版本不仅能够识别肿瘤PD-L1,还能阻断其制动机制,从而引导CAR-T细胞到达肿瘤表面,攻击并杀死肿瘤细胞。”
“想象一下,如果你想在海洋中找到一种非常特殊的鱼——那将非常困难,”刘说。“但现在有了我们开发的定向进化平台,我们就有办法找到具有正确功能的特定蛋白质了。”
研究团队目前正在探索如何优化这些蛋白质,以便在临床应用之前创造出更精准、更有效的CAR-T细胞。这还包括将这些蛋白质与王实验室突破性的聚焦超声应用相结合,以远程控制CAR-T细胞,使其仅在肿瘤部位被激活。
王教授说:“我们现在拥有所有这些基因工具来操纵、控制和编程这些免疫细胞,使其拥有如此强大的功能。我们希望创造新的方法来引导它们的功能,以用于特别具有挑战性的实体瘤治疗。”

