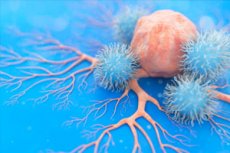
当细胞变成肿瘤细胞时,其代谢会发生巨大变化。巴塞尔大学和巴塞尔大学医院的研究人员证明,这些变化会留下痕迹,可以作为癌症免疫治疗的靶点。
癌细胞以涡轮模式运作:它们的新陈代谢被设定为快速繁殖,同时它们的遗传物质也被不断复制并转化为蛋白质。
巴塞尔大学和巴塞尔大学医院的Gennaro De Libero教授领导的研究人员报告称,这种快速代谢会在肿瘤细胞表面留下痕迹,可被特定的免疫细胞读取。该研究小组的研究成果发表在《科学免疫学》杂志上。
大约10年前,与德·利贝罗合作的免疫学家发现了这种被称为MR1T细胞的免疫细胞。这种此前未知的T细胞能够攻击并摧毁肿瘤细胞。从那时起,该团队一直在研究这些细胞,将其作为针对各种癌症的新型免疫疗法的潜在工具。
修改 DNA 和 RNA 构建块该团队已经成功破译了 T 细胞如何识别退化细胞:癌细胞改变的代谢会产生一种出现在这些退化细胞表面的某种分子。
“这些分子是 DNA 和 RNA 的化学修饰组成部分,是由三种重要代谢途径的变化引起的,”德利贝罗解释道。
参与这项研究的 Lucia Mori 博士补充道:“癌细胞的新陈代谢发生了显著改变,这使得它们能够被 MR1T 细胞识别。”
在之前的研究中,研究人员已经发现这些T细胞能够识别一种存在于所有细胞表面的蛋白,即MR1。MR1就像一个“银盘”,将细胞内部的代谢废物输送到细胞表面,以便免疫系统检查细胞是否健康。
“癌细胞中的几种代谢途径发生了改变。这会产生特别可疑的代谢产物,从而引起MR1T细胞的注意,”该研究的第一作者Alessandro Vacchini博士解释道。
研究人员的下一步是更详细地研究这些特征代谢物如何与MR1T细胞相互作用。他们的长期愿景是:在未来的治疗中,患者的T细胞可以被重新编程和优化,以识别和攻击这些癌症特异性分子。

