Simone Steger 团队的这一发现或将助力研发一种治疗最严重利什曼病的疗法。利什曼病是一种热带疾病,全球患病人数日益增多。每年新增病例约 70 万至 100 万例。其病原体是一种利什曼原虫属的原生动物寄生虫,通过蚊虫叮咬传播给人类。利什曼病有三种临床类型,其中内脏型最为严重。
如果不及时治疗,内脏利什曼病几乎总是致命的。大多数病例发生在孟加拉国、巴西、埃塞俄比亚、印度、尼泊尔和苏丹。
英国国家科学研究所 (INRS) 的 Steger 教授及其团队与 INRS 和麦吉尔大学的其他研究人员合作,观察到了与慢性内脏利什曼病相关的一种令人惊讶的免疫机制。这一发现可能为该疾病的新治疗策略迈出重要一步。他们的研究成果发表在《细胞报告》杂志上。
在许多感染中,CD4 T细胞在宿主的防御中发挥着关键作用。然而,在利什曼病等慢性感染中,维持功能性CD4细胞计数变得至关重要,因为免疫系统会持续被激活以应对病原体。
新的免疫防御者然而,斯蒂格教授在印度国家科学研究院阿芒-弗拉皮尔生物技术与健康研究中心的实验室中进行的研究表明,这些细胞可能有多种方法来维持其活力。
“我们在感染了导致内脏利什曼病的寄生虫的小鼠体内发现了一种新的CD4细胞群。这些T细胞具有有趣的特性,”Steger教授说。
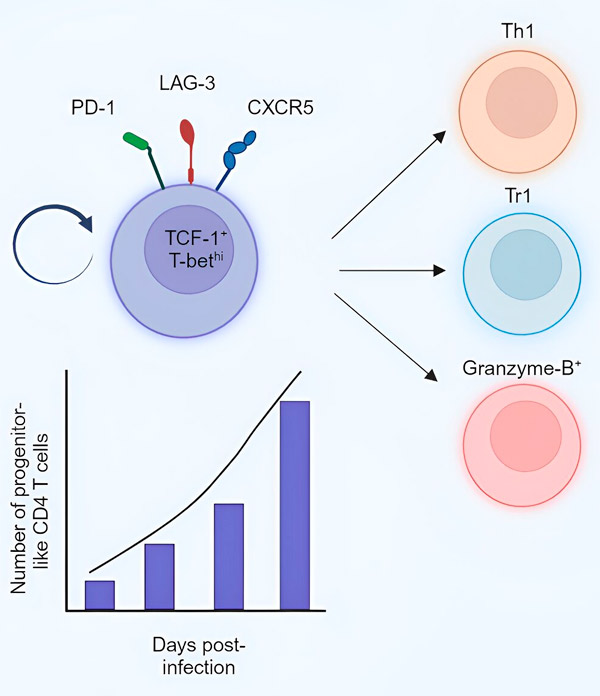
通过监测这些新细胞,科学家们注意到它们的数量在疾病的慢性期增加,并且像祖细胞一样,它们能够自我更新或分化为负责消灭寄生虫的其他效应细胞或抑制宿主反应的调节细胞。
Steger教授指出,CD4 T细胞通常会从“幼稚”CD4 T细胞分化为效应细胞。但在慢性感染期间,由于需要不断生成效应细胞,幼稚CD4 T细胞会变得超负荷,并可能被耗尽。
“我们认为,在内脏利什曼病的慢性期,我们鉴定出的新细胞群负责生成效应细胞和调节细胞。这将使宿主能够防止针对特定抗原的现有幼稚CD4 T细胞库的耗竭,”该研究的第一作者、博士生Sharada Swaminiathan解释说。
INRS 团队发现的新淋巴细胞群可能成为重要的免疫增强剂,取代超负荷的幼稚 CD4 T 细胞。
斯蒂格教授说:“如果我们能够弄清楚如何引导这种新的淋巴细胞群分化为防御效应细胞,它可能有助于宿主摆脱利什曼原虫。”
治疗其他感染的方法?该研究还提到,在感染淋巴细胞性脉络丛脑膜炎病毒的小鼠和携带肠道蠕虫H. polygyrus的小鼠中也发现了类似的细胞。因此,这种细胞群可能存在于其他慢性感染或其他慢性炎症环境中。
这一事实为Steger教授团队的发现开辟了更广阔的前景。“如果我们的假设正确,这些细胞不仅可以用于治疗内脏利什曼病,还可以用于治疗其他慢性感染。”研究人员总结道。

