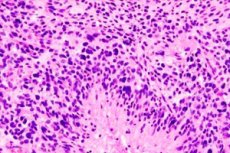
佛罗里达大学的研究人员首次进行了人体临床试验,结果表明他们的 mRNA 癌症疫苗可以快速重新编程免疫系统,以攻击最具侵袭性和致命性的脑肿瘤——胶质母细胞瘤。
这项在四名成年患者身上进行的试验结果,与在10只患有自然脑瘤的宠物狗身上获得的类似结果相符。由于没有其他治疗选择,这些宠物狗的主人同意参与试验。这项突破性进展目前正在针对患有脑癌的儿童进行I期临床试验。
该研究结果发表在《细胞》杂志上,代表了一种利用免疫系统对抗难治性癌症的潜在新方法,即使用改良的 mRNA 技术和脂质纳米颗粒,类似于 COVID-19 疫苗,但有两个主要区别:使用患者自身的肿瘤细胞来制造个性化疫苗,以及疫苗内部的新型、复杂的输送机制。
“我们不是注射单个粒子,而是注射像洋葱袋一样相互缠绕的粒子簇,”资深作者、佛罗里达大学健康中心儿科肿瘤学家、开发了这种新疫苗的医学博士、哲学博士Elias Sayur说道。与其他免疫疗法一样,这种疫苗会“训练”免疫系统将肿瘤识别为异物。
萨尤尔说:“最令人印象深刻的发现之一是,这种通过静脉注射的新方法能够迅速引发强大的免疫反应来排斥肿瘤。”
“在不到 48 小时的时间里,我们就能看到这些肿瘤从‘冷’状态(免疫细胞活动很少)转变为‘热’状态(免疫反应非常活跃)。”
胶质母细胞瘤是最具破坏性的疾病之一,平均生存期约为15个月。标准治疗包括手术、放射治疗和化疗联合治疗。
这项新出版物是七年研究的成果,首先从临床前小鼠模型开始,然后对 10 只患有晚期脑癌的宠物狗进行临床试验,并在主人同意的情况下与佛罗里达大学兽医学院合作进行。
在使用个性化 mRNA 疫苗治疗宠物狗后,Sayur 的团队进行了小规模、经 FDA 批准的临床试验,以确保安全性并测试可行性,然后再扩大到更大规模的试验。
在四名患者中,研究人员从每位患者切除的肿瘤中提取了名为RNA的遗传物质,然后将mRNA扩增并包装到高科技生物相容性脂质纳米颗粒中,使肿瘤细胞在重新注入血液并触发免疫反应时“看起来”像危险的病毒。疫苗针对每位患者进行了个性化定制,以最大限度地发挥其独特的免疫系统功能。
佛罗里达大学临床和转化研究所所长、佛罗里达大学脑肿瘤免疫治疗项目主任、论文共同作者杜安·米切尔 (Duane Mitchell) 医学博士表示:“证明以这种方式制造的 mRNA 癌症疫苗能够在小鼠、患有自然癌症的宠物狗和患有脑癌的人类患者身上引发类似且强烈的反应,是一项非常重要的发现。”
虽然现在评估疫苗的临床效果还为时过早,但患者要么比预期更长时间地无病生存,要么比预期更长寿。
这 10 只宠物狗的平均存活时间为 139 天,而患有这种疾病的狗的平均存活时间为 30-60 天。
下一步,在 FDA 和儿童癌症基金会 CureSearch 的支持下,将进行扩大的第一阶段临床试验,最多有 24 名成人和儿童参与,以确认结果。
一旦确认最佳安全剂量,约有 25 名儿童将参加第二阶段研究。
“我希望这能成为治疗病人的新范例,调节免疫系统的新平台,”Sayur说。
Sayur 和 Mitchell 拥有与疫苗相关的专利,这些专利正在向佛罗里达大学成立的生物技术公司 iOncologi Inc. 申请授权。

