B 细胞可以通过释放某些细胞因子(控制免疫细胞生长和活动的小蛋白质)来控制髓细胞反应,挑战了之前认为只有 T 细胞协调免疫反应的观念。
对于多发性硬化症(MS)患者,B 细胞异常活跃的呼吸会刺激髓细胞和 T 细胞的促炎反应,导致它们攻击覆盖神经纤维的保护鞘(髓鞘),从而造成神经损伤和 MS 症状。
一类名为布鲁顿酪氨酸激酶 (BTK) 抑制剂的新型药物或许能够逆转这种异常的 B 细胞呼吸,并阻断导致多发性硬化症 (MS) 发作的信号。这项由宾夕法尼亚大学佩雷尔曼医学院领导的研究发表在《科学免疫学》杂志上。
宾夕法尼亚大学神经病学教授兼神经炎症和神经治疗中心主任阿米特·巴奥尔博士说:“专家们以前认为,T 细胞是其他类型免疫细胞反应的主要协调者,而 MS 主要是由过度活跃的 T 细胞引起的。”
“这项研究强调了不同细胞类型如何相互作用确实很重要,并且髓系调节 B 细胞在免疫系统中发挥的作用比我们想象的要积极得多。”
健康的免疫系统会持续地对刺激作出反应,激活或抑制免疫反应,部分是通过释放各种细胞因子来指示其他类型的细胞如何反应。通常情况下,每种免疫反应都会引发反作用,这种持续的“推拉”作用有助于维持免疫反应之间的适当平衡。
这样,人体免疫系统一方面可以对感染做出反应,另一方面也可以确保免疫系统不会过度活跃并对身体造成伤害,就像多发性硬化症等自身免疫性疾病中发生的情况一样。
在这项研究中,研究人员使用了人类样本和小鼠 MS 模型来证明,不仅 MS 中的 B 细胞和 T 细胞之间的细胞因子信号出现问题,而且 MS 患者的 B 细胞还会产生异常的细胞因子谱,导致髓系细胞产生炎症反应。
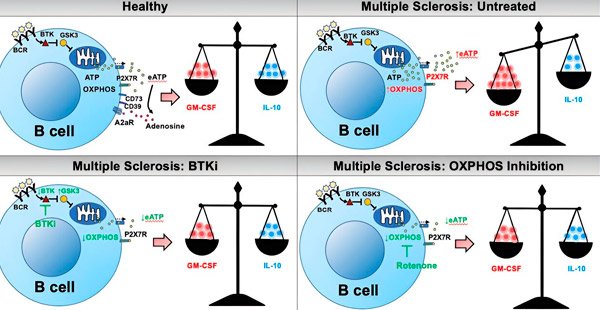
他们发现,所有这些作用都可以追溯到B细胞中一种名为氧化磷酸化(一种线粒体呼吸作用)的代谢失调。研究人员发现,正常的B细胞能够分解氧气并释放化学能量信号,这些信号会触发B细胞自身以及髓系细胞的进一步反应,指示它们发起促炎或抗炎反应。
然而,当 B 细胞代谢过度活跃时(如多发性硬化症 (MS) 的情况),信号会导致异常的髓系和 T 细胞反应,这与多发性硬化症(MS) 症状的爆发有关。
B细胞对细胞因子产生的代谢调节:对多发性硬化症(MS)发病机制和治疗的意义。来源:Science Immunology (2024)。DOI:10.1126/sciimmunol.adk0865
Bar-Or 说:“治疗多发性硬化症的一种令人兴奋的新方法可能是部分抑制 B 细胞的呼吸,这可以阻止驱动炎症和多发性硬化症活动的免疫细胞之间的级联相互作用。”
作者此前已证明,一类名为 BTK 抑制剂的新型药物就能做到这一点。这些药物可以减缓过度活跃的 B 细胞呼吸,并“镇静”多发性硬化症患者的 B 细胞,使它们不会分泌出引发髓系细胞和 T 细胞异常促炎反应的异常细胞因子。
现有的多发性硬化症 (MS) 疗法,例如抗 CD20 疗法,会消耗 B 细胞。然而,由于 B 细胞被破坏,患者的免疫系统可能会受到损害,使其难以对感染或疫苗接种做出反应。相比之下,BTK 抑制剂不会消耗 B 细胞,而是纠正代谢异常,使 B 细胞不太可能触发其他细胞的促炎反应。

