
与之前的研究一致,西奈山医学中心伊坎医学院的研究人员表明,与健康人相比,海洛因使用障碍患者在执行冲动抑制任务时,前部和背外侧前额叶皮质 (PFC) 的活动减少。
值得注意的是,15周的药物辅助治疗(包括辅助性团体治疗)改善了一组海洛因使用障碍患者在冲动抑制任务中受损的前部和背外侧PFC功能。这表明,在接受干预后,海洛因使用障碍患者的冲动控制和PFC功能呈现出时间依赖性的恢复。
该研究发表在《自然心理健康》杂志上。
成年人因阿片类药物(包括海洛因)过量服用而死亡的人数持续快速上升。冲动控制——即即使面临严重的负面后果并有戒毒意愿,仍能抑制吸毒等不良行为的能力——在吸毒成瘾者中存在缺陷,其前额叶皮质(负责自我控制过程的大脑区域)功能失活。
本研究招募了26名正在接受药物辅助治疗的海洛因使用障碍住院患者和24名人口统计学匹配的健康参与者,进行功能性磁共振成像 (fMRI) 的纵向研究。住院海洛因使用障碍患者的参与者完成了两次 fMRI 治疗,两次治疗间隔15周,而健康参与者则完成了相同时间间隔的 fMRI 治疗。
在功能磁共振成像(fMRI)检查中,受试者执行了停止信号任务,这是一项经过充分验证的工具,用于评估冲动控制过程中的大脑功能。在任务中,受试者对箭头刺激做出反应,并在箭头周期性地变红(停止信号)时抑制反应。除了15周住院治疗后PFC区域活动增加外,海洛因使用障碍患者的活动增加还与停止信号任务表现的提高相关。
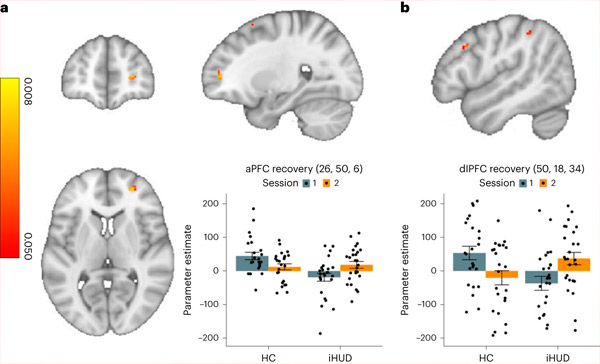
与HC组相比,iHUD组负责冲动控制的大脑活动从基线到随访时间有所增加。a,b, iHUD组在成功和不成功停止冲动时,右侧aPFC(a)和右侧dlPFC(b)的活动从基线到随访时间显著增加。来源:《自然心理健康》(2024)。DOI:10.1038/s44220-024-00230-4
“总体而言,我们的研究结果表明,前部和背外侧 PFC 区域可能适合有针对性的干预,可以加速它们在冲动控制过程中的恢复,这可能对未来的治疗具有实际意义,”高级博士后研究员兼论文主要作者 Ahmet O. Ceceli 博士说。
“需要更多研究来确定住院治疗中是否存在显著促进病情改善的特定因素,并考察其他具体因素。例如,我们的研究团队计划测试我们在本研究中观察到的康复效果是否源于作为额外团体治疗干预一部分的正念干预,”西奈山伊坎医学院精神病学和神经科学教授、该论文的资深作者丽塔·Z·戈德斯坦博士说道。

