Antibacterial protein - a new target for the treatment of pancreatic cancer
最近審查:14.06.2024
Immunotherapy represents new hope in the fight against cancer, but not all tumors respond to this treatment. Pancreatic cancer is a type of tumor that does not respond to current approved drugs and is therefore fatal for 9 out of 10 people diagnosed.
For this reason, it is necessary to find new targets to attack resistant cells, such as cancer stem cells, which are mainly responsible for tumor initiation, metastasis formation and treatment resistance.
A recent study by the Spanish National Research Council (CSIC), published in the journal Gut, describes how pancreatic cancer stem cells use the antibacterial protein PGLYRP1 to evade immune systems and protect yourself from early destruction.
When this protein is removed, the body's defense mechanisms are able to recognize tumor cells and destroy them. This will allow the development of new immunotherapies that will target the root cause of pancreatic cancer and lead to improved therapies in the future.
The study was jointly carried out by three scientists: Bruno Sainz, head of the group for research on cancer stem cells and fibroinflammatory microenvironment at the Biomedical Research Institute of Sols-Morreale (IIBM), CSIC-UAM and the group on biomarkers and personalized approaches to cancer treatment (BIOPAC) at the Ramon y Cajal Institute for Health Research (IRYCIS); Christopher Heschen from the Candiolo Cancer Institute (IRCCS) in Italy and Susanna García Silva, a scientist from the Spanish National Cancer Research Center (CNIO).
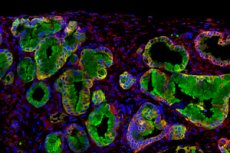
Over the past ten years, these three scientists have led a joint project in which they identified a population of pancreatic cancer stem cells (CSCs) present in mouse models of the disease. These cells, known as the tumor root, are responsible for relapses of the disease after treatment with chemotherapy or radiotherapy.
Interestingly, pancreatic cancer is also one of the most resistant tumors to immunotherapy. However, until now, the mechanisms by which CSCs evade destruction by the immune system remained unclear.
As a result of this collaboration, peptidoglycan recognition protein 1 (PGLYRP1) was identified as one of the causes of immune system evasion by CSCs using sophisticated mouse models and patient samples. This work is the first to describe the role of this protein in pancreatic cancer, which is produced in excess in stem cells. This discovery lays the groundwork for developing a treatment against it.
Potential therapy against the root cause of pancreatic cancer
“When we eliminate PGLYRP1 from tumor cells, we see that the immune system responds by attacking them, preventing primary tumor formation and metastatic spread,” explains Sainz, group leader at IIBM. “We are now developing therapies to block or eliminate this protein with the hope of being able to combine them with current treatments to more effectively attack and eliminate cancer stem cells, the root of the tumor,” he adds.
Over the past four years, Juan Carlos Lopez-Gil, the first author of the paper, has been able to decipher why CSCs produce this protein in pancreatic cancer. He says: “We saw that immune cells try to kill tumor cells by producing tumor necrosis factor, but PGLYRP1 is very similar to this factor and interacts with the same receptor, blocking it.”
For the researcher, this means that “CSCs protect themselves by using an incomplete key (PGLYRP1) to block the lock (the receptor) and thus avoid death caused by tumor necrosis factor (the complete key).”
What surprises the researchers is that the protein used by our immune system to fight bacteria is used by pancreatic cancer to protect itself from these same defense mechanisms. “The priority going forward will be to understand the mechanisms by which tumor cells hijack physiological processes to ‘re-educate’ the tumor environment and make it react against them,” says co-author Garcia-Silva.

