Study Identifies Linked Biological Pathways Causing Skin Inflammation in Psoriasis
最近審查:14.06.2024

New research has identified a biological pathway—a set of related reactions in the body—that leads to the inflammation seen in the skin disease psoriasis. The study authors say these findings could lead to improved treatments for all inflammatory skin diseases, including atopic and allergic dermatitis, as well as a type of boil called pustular hidradenitis.
Inflammation is the body's natural response to irritation and infection, but when left uncontrolled, it can lead to the reddish, scaly, itchy lesions characteristic of these skin conditions.
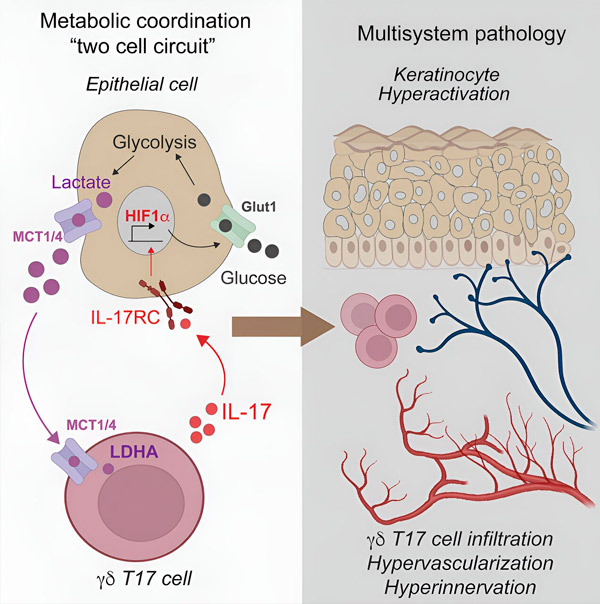
Leading researchers from NYU Langone Health have discovered that the interleukin-17 (IL-17) pathway, whose activity is blocked by existing anti-inflammatory drugs, activates a protein called hypoxia-inducible factor 1-alpha (HIF-1-alpha) in psoriasis. The researchers say IL-17 has long been known to be active in inflammation, but the role of HIF-1alpha has been unclear until now.
The team also found that HIF-1 alpha allows inflamed skin cells to more actively break down sugar for energy, supporting their metabolism and leading to the production of a byproduct called lactate. When inflammatory T cells consume lactate, it triggers the production of IL-17, increasing inflammation.
The results showed that in skin tissue samples from people with psoriasis, measures of gene activity around IL-17 and HIF-1-alpha were similar, suggesting that these factors are related. Experiments on mice in which psoriasis was induced showed that subsequent treatment with an experimental drug that blocks the action of HIF-1-alpha, called BAY-87-2243, resolved the inflammatory skin lesions.
In addition, skin samples from 10 patients successfully treated with the anti-inflammatory drug etanercept showed decreased activity of both IL-17 and HIF-1alpha, indicating that blocking IL-17 also blocks HIF-1alpha. Alpha.
"Our results indicate that HIF-1alpha activation is a key driver of the metabolic dysfunction seen in psoriasis and that its action is triggered by IL-17, another key inflammatory signaling molecule," said lead study author Shruti Naik, Ph.D., Associate Professor, NYU Grossman School of Medicine, Departments of Pathology and Medicine, and Ronald O. Perelman Department of Dermatology.Additional experiments were conducted on skin samples from five patients with psoriasis whose healthy and inflamed skin were separately treated with either BAY-87-2243 or an existing combination of topical drugs (calcipotriene and betamethasone dipropionate).
The researchers then compared differences in inflammatory gene activity as a measure of impact and found that the HIF-1-alpha inhibitor had a greater impact than existing topical drugs. Specifically, skin samples that responded to HIF-1alpha therapy had 2,698 differentially expressed genes, while samples treated with standard therapy had 147 differentially expressed genes.
Genetic analysis of skin samples from another 24 psoriasis patients treated with the IL-17A blocking drug secukinumab showed only a decrease, not an increase, in the activity of HIF-1 alpha-related genes compared with the activity of HIF-1 genes -alpha in nine healthy patients without psoriasis. The researchers believe that this indicates that blocking the action of HIF-1-alpha is dependent on blocking IL-17.
Additional experiments in mice showed that blocking the absorption of sugar (glucose) in the skin slowed the growth of psoriatic disease by limiting glucose metabolism, or glycolysis. The number of inflammatory T cells and IL-17 levels decreased. It was also found that levels of lactate, a major byproduct of glycolysis, in psoriatic skin cell cultures decreased after exposure to the glycolysis-inhibiting drug 2-DG.
Directly targeting lactate production in psoriatic mice using a skin cream containing lactate dehydrogenase, which degrades lactate, also slowed disease progression in the skin, with a decrease in the number of inflammatory gamma delta T cells and a decrease in IL-17 activity. Gamma delta T cells have been shown to take up lactate and use it to produce IL-17.
"Our findings suggest that blocking the action of HIF-1alpha or its glycolytic metabolic support may be an effective therapy for curbing inflammation," added Naik, who is also associate director of the Judith and Stuart Colton Center for Autoimmunity at NYU Langone.
p>"Evidence of downregulation of HIF-1alpha, or its suppression, may also serve as a biomarker, or molecular sign, that other anti-inflammatory therapies are working," said Dr. Jose W. Sher, study co-author and assistant professor of medicine at the school of medicine. Grossman at NYU.
Scher, who is also director of the Psoriatic Arthritis Center and the Judith and Stuart Colton Center for Autoimmunity at NYU Langone, says the team plans to develop experimental drugs that can block the effects of HIF-1 alpha and lactate in the skin "to end the vicious cycle of IL-17-induced inflammation in skin diseases. Our study significantly expands the possibilities for therapeutic options."Nike stresses that while many available treatments for psoriasis, including steroids and immunosuppressive drugs, reduce inflammation and symptoms, they do not cure the disease. She said more experiments are needed to clarify which experimental drug works best at inhibiting HIF-1alpha before clinical trials can begin. Naik and lead study co-authors Ipsita Subudhi and Piotr Konieczny have applied for a patent (U.S. Application number 63/540,794) for a therapy for inflammatory skin diseases based on their work on inhibiting HIF-1alpha.
It is estimated that more than 8 million Americans and 125 million people worldwide suffer from psoriatic disease. This condition affects both men and women equally.
The results were published in Immunity magazine.

