Drug discovered that may delay the onset of Alzheimer's and Parkinson's disease
最近審查:14.06.2024

A researcher in the Department of Surgery at the Keck School of Medicine of the University of Southern California (USC) has discovered a potential breakthrough in delaying the onset of Alzheimer's and Parkinson's diseases and treating hydrocephalus. Young-Kwon Hong, Ph.D., director of basic research in the Department of Surgery, and his team have developed a drug that may help clear fluid and cellular debris from the brain.
Like the body, the brain has its own lymphatic system, which removes cellular waste. "It's like a sewer system, and it has to drain well for everything to work and stay clean," Hong explained. When the brain's lymphatic system does not drain properly, fluid and debris can accumulate. Fluid accumulation means there is less room for cerebrospinal fluid, which cushions and nourishes the brain.
Hydrocephalus is an accumulation of fluid in the brain. This fluid can put pressure on both the skull and the brain itself. Because the development of the skull bones in children is not complete, hydrocephalus can cause deformation of the skull and possible damage to the growing brain.
In adults, hydrocephalus causes the brain to press against the hardened skull, leading to headaches and symptoms ranging from vision problems to difficulties with coordination and cognitive problems. Parkinson's and Alzheimer's have many causes, but the buildup of waste and plaque in the brain is a significant factor in each.
Benefit of Large Pipes Hong's team theorized that they could speed up the drainage of fluid and waste from the brain. “Think of a kitchen sink that drains too slowly because of a two-inch pipe,” he said. "We can offer you a four-inch diameter pipe." Hong's team first developed the idea of manually stimulating the drainage process, and then they developed a compound that causes an increase in the diameter of lymphatic vessels.
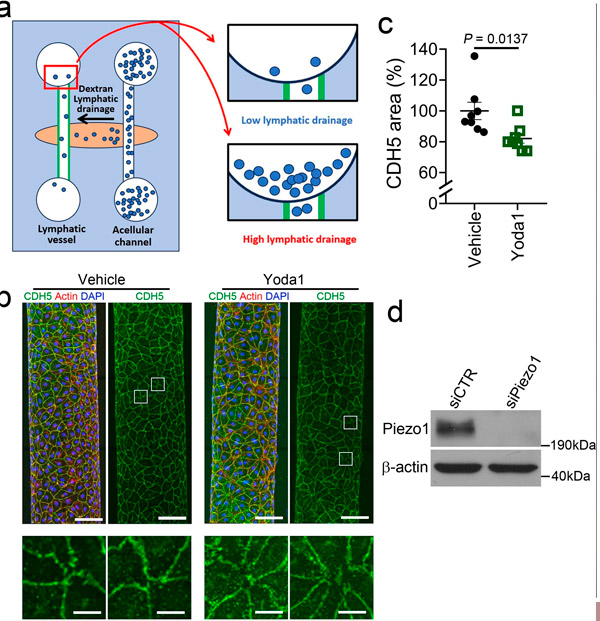
Piezo1 activation reduces CDH5-stained area and increases drainage in simulated lymphatic vessels on a polydimethylsiloxane (PDMS) chip. (a) Schematic illustration of the 3D model of lymphatic vessels used in this study. (b) Fluorescence confocal images of engineered lymphatic vessels stained for F-actin and CDH5. (c) Relative area of cell junctions stained with CDH5. (d) Western blot analysis confirming efficient reduction of Piezo1 levels in lymphatic endothelial cells (LECs) prepared for drainage measurements. Source: Nature Neuroscience (2024). DOI: 10.1038/s41593-024-01604-8
Hong's research was published in Nature Neuroscience in March of this year, and he and his team continue to work on this exciting development.
The unusual aspect of this story is that, despite decades of experience in medical and surgical research, Hong had no previous neuroscientific research—all of his work focused on areas below the neck. He found inspiration for this project in church.
One of his congregation members had adult-onset hydrocephalus and experienced sudden loss of vision while driving on the freeway. When Hong heard about this incident, he felt he had to help. "I felt a spiritual call. I had to do something."
Hong noted that despite his first experience in neuroscientific research, everything came together and worked surprisingly well. And, of course, there is the potential to help millions of people around the world. "It was incredible," he said. "It's the perfect combination of science and faith."

