在最近发表在《BMJ 健康与护理信息学》杂志上的一项研究中,研究人员评估了使用面部红外热成像 (IRT) 预测冠心病 (CHD) 的可行性。
冠心病 (CHD) 是主要死因之一,在全球范围内造成沉重的负担。准确诊断冠心病对于护理和治疗至关重要。目前,验前概率 (PTP) 评估工具用于确定患者罹患冠心病的可能性。然而,这些工具存在主观性强、通用性有限和准确性中等的问题。
尽管额外的心血管测试(冠状动脉钙化评分和心电图)或整合额外实验室标志物和风险因素的复杂临床模型可能会改善概率估计,但仍存在与时间效率、程序复杂性和可用性有限相关的问题。
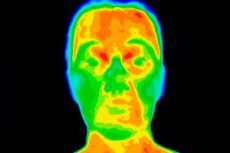
IRT 是一种非接触式表面温度检测技术,在疾病评估方面显示出良好的应用前景。它可以通过皮肤温度模式检测炎症和异常血流。研究表明,IRT 信息与动脉粥样硬化性心血管疾病及相关疾病之间存在关联。
在本研究中,研究人员评估了使用面部IRT温度数据预测冠状动脉疾病(CAD)的可行性。研究对象为接受冠状动脉CT血管造影(CCTA)或侵入性冠状动脉血管造影(ICA)的成年人。训练有素的人员在CCTA或ICA检查前采集基线数据并进行IRT采集。
使用电子病历获取更多信息,包括血液生化、临床病史、风险因素和CAD筛查结果。每位参与者选择一张IRT图像进行分析和处理(统一调整大小、转换为灰度图和裁剪背景)。
该团队利用先进的深度学习算法开发了IRT图像模型。为了进行比较,他们开发了两个模型:一个是包含患者年龄、性别和症状特征的PTP(临床基线)模型;另一个是混合模型,分别结合了IRT和PTP模型中的临床信息。
我们进行了多项解释分析,包括遮挡实验、高光图可视化、剂量反应分析以及替代 CAD 标签预测。此外,我们从 IRT 图像中提取了各种 IRT 表特征,并按全脸和感兴趣区域 (ROI) 级别进行分类。
总体而言,提取的特征分为一阶纹理特征、二阶纹理特征、温度特征和分形分析特征。XGBoost 算法整合了这些提取的特征,并评估了它们对冠心病的预测价值。研究人员评估了使用所有特征和仅使用温度特征进行预测的性能。
2021年9月至2023年2月期间,共筛查了893名接受CCTA或ICA检查的成年人。其中,纳入460名参与者,平均年龄58.4岁;27.4%为女性,70%患有冠状动脉疾病(CAD)。CAD患者的年龄和危险因素患病率均高于无CAD患者。IRT-图像模型显著优于PTP模型。
然而,混合模型和IRT图像模型的性能差异并不显著。仅使用温度特征或所有提取的特征均具有更优的预测性能,这与IRT图像模型一致。在整个面部层面,整体左右温差的影响最大,而在ROI层面,左下颌的平均温度的影响最大。
在遮挡不同的ROI时,IRT-图像模型的性能下降程度各不相同。遮挡上唇和下唇区域的影响最大。此外,IRT-图像模型在预测与冠状动脉疾病(CAD)相关的替代指标(例如高脂血症、吸烟、体重指数、糖化血红蛋白和炎症)方面表现良好。
本研究证明了利用面部IRT温度数据预测CAD的可行性。IRT图像模型的表现优于指南推荐的PTP模型,凸显了其在CAD评估中的潜力。此外,将临床信息纳入IRT图像模型并未带来额外的改进,这表明提取的IRT信息本身就包含了与CAD相关的重要信息。
此外,利用可解释的IRT表格特征验证了IRT模型的预测价值,这些特征与IRT图像模型相对一致。这些特征还提供了预测冠心病(CHD)的重要方面的信息,例如面部温度对称性和分布不均匀性。未来仍需开展更大样本、更多样化人群的研究进行验证。

